Triple-Negative Breast Cancer (TNBC): Causes, Diagnosis, and Treatment
Learn about triple-negative breast cancer (TNBC), a fast-growing and aggressive type of breast cancer. Explore its risk factors, symptoms, diagnosis, and current treatment options including surgery, chemotherapy, and targeted therapies.
Triple-Negative Breast Cancer (TNBC)
Triple-Negative Breast Cancer (TNBC) grows and spreads more rapidly compared with other types of invasive breast cancer.
In most other invasive breast cancers, tumor cells express estrogen receptors (ER), progesterone receptors (PR), and/or human epidermal growth factor receptor 2 (HER2). In contrast, TNBC is defined by the absence of ER and PR expression and the lack of HER2 overexpression.
Triple-negative breast cancer (TNBC) accounts for approximately 15–20% of breast cancer cases worldwide and is the second leading cause of cancer-related deaths. It is characterized by aggressiveness, a high chance of metastasis, early recurrence, and an overall poor prognosis.
Nearly 40% of patients with stage I–III TNBC experience disease recurrence within the first 2–3 years following treatment.
Compared with patients with non-TNBC breast cancer, those with TNBC have a higher risk of developing distant organ metastases, particularly to the brain and lungs.
Furthermore, when compared with patients with hormone receptor–positive breast cancer, TNBC patients have an average 5-year relative survival rate of approximately 77%, which is 8–16% lower
Triple-Negative Breast Cancer Risk Factor
Age-TNBC is more commonly diagnosed in younger women, particularly those under 40 years of age, and in individuals with BRCA1 mutations.
Race- TNBC affects African American women, who experience higher mortality rates compared with White women.
Related Article: Rare Type of Breast Cancer
Triple-Negative Breast Cancer Symptoms
Symptoms are similar to other breast cancer symptoms:
- Lump or mass in your breast
- Breast pain or nipple pain
- Dimpled breast skin
- Nipple turning inward
- Nipple discharge
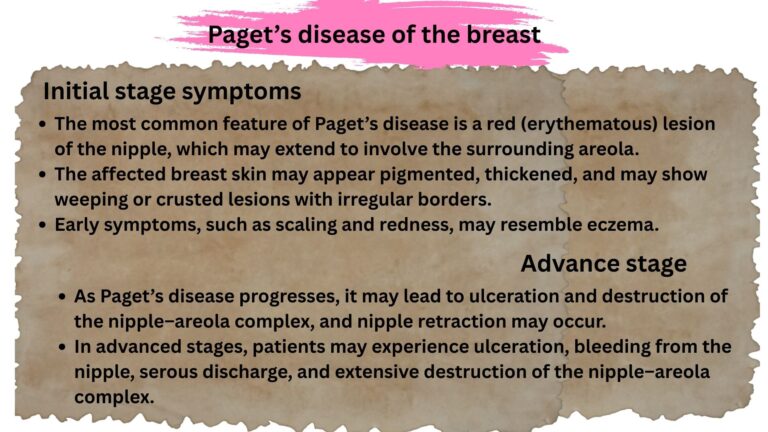
- Dryness, flaking, thickened or redness in nipple or breast skin
- Swelling in all or part of your breast
- Swollen lymph nodes under arm or near collarbone.
Why TNBC treatment is very difficult?
In many other types of breast cancer, treatment commonly involves medications that target HER2, estrogen, or progesterone receptors. However, such targeted therapies are ineffective in triple-negative breast cancer (TNBC) because TNBC cells lack HER2 expression and do not express estrogen or progesterone receptors. As a result, HER2-targeted drugs and hormonal therapies do not work in TNBC.
Because of the absence of these therapeutic targets, TNBC generally has fewer treatment options and can be more challenging to treat than other forms of breast cancer. TNBC also tends to grow and spread more rapidly, which has led many clinicians to consider it a more aggressive subtype. However, tumor aggressiveness is influenced not only by subtype but also by factors such as tumor size, stage, and molecular characteristics.
Despite having fewer targeted treatment options, several effective therapies for TNBC do exist, including chemotherapy and newer approaches such as immunotherapy. Ongoing research is focused on developing novel treatments and optimizing existing therapies to better tailor care to the specific biology and clinical circumstances of each patient.
Triple-Negative Breast Cancer Diagnosis
The main diagnostic methods for TNBC include mammography, ultrasound, magnetic resonance imaging (MRI), biopsy, and histopathological analysis.
Mammography has low sensitivity for detecting TNBC, with an accuracy of only 39.8%.
Ultrasound is mainly useful for distinguishing between benign and solid lesions but has limited ability to identify malignant features.
MRI is more sensitive than mammography and ultrasound.
Biochemical testing is still required to confirm the diagnosis, treatment decisions, and prognosis prediction. Among these approaches, biochemical detection shows strong potential for early screening and precise treatment at a larger scale and lower cost.
Triple-Negative Breast Cancer Treatment
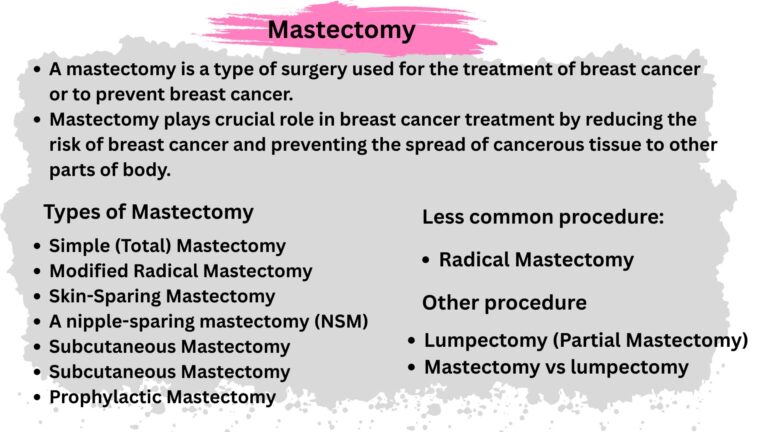
Surgery
TNBC is primarily treated with surgery. Depending on the stage of the cancer, either a lumpectomy (removal of the tumor along with a small margin of surrounding tissue) or a mastectomy (removal of the entire breast) may be performed.
Surgery is often combined with chemotherapy, which may be given before surgery (neoadjuvant) or after surgery (adjuvant).
Hormonal therapies are not effective in TNBC due to the absence of hormone receptors. Depending on the clinical condition and patient characteristics, surgery may be used alone or in combination with chemotherapy to improve treatment outcomes.
Radiation
Radiation therapy is often used after mastectomy to eliminate any remaining cancer cells in the breast or lymph nodes. However, recurrence occurs in approximately 7–12.6% of patients within five years after radiation therapy, and resistance to radiation can develop. Therefore, radiotherapy is commonly combined with immunotherapy to improve treatment outcomes.
Chemotherapy
Chemotherapy for TNBC depends on the patient and the stage of the disease. Because TNBC is aggressive, treatment usually involves a combination of chemotherapy and surgery to effectively kill cancer cells throughout the body.
Chemotherapy is the standard treatment for TNBC and commonly includes drugs are anthracyclines (e.g., doxorubicin) and taxanes (e.g., paclitaxel), which may be given before surgery (neoadjuvant) or after surgery (adjuvant).
Targeted Therapy
PARP Inhibitors
Breast cancer patients with BRCA mutation, PARP inhibitor is used to treat cancer.
Androgen Receptor Antagonists
TNBC lacks the common hormonal receptors estrogen receptor (ER), progesterone receptor (PR), and HER2. However, other hormone receptors, such as glucocorticoid receptors and androgen receptors (AR), may be expressed in TNBC.
Androgen receptors play an important role in TNBC cell proliferation, invasion, migration, and apoptosis, thereby contributing to disease progression. Therefore, therapies targeting AR, such as androgen receptor inhibitors, represent a promising treatment option for TNBC.
EGFR Inhibitors
Epidermal growth factor receptor (EGFR) is a promising target for cancer therapy. It is a cell-surface tyrosine kinase receptor involved in regulating cell proliferation, invasion, angiogenesis, and survival. High EGFR expression is associated with larger tumors, poor differentiation, and worse clinical outcomes in breast cancer. Therefore, targeting or suppressing EGFR may improve treatment outcomes in TNBC.
VEGF Inhibitors
Vascular endothelial growth factor (VEGF) promotes tumor growth and the formation of new blood vessels and plays an important role in breast cancer progression. High VEGF levels in TNBC are associated with poor clinical outcomes, regardless of tumor size or grade. Because angiogenesis is essential for tumor growth, bevacizumab, a monoclonal antibody targeting the VEGF pathway, has been investigated in TNBC and has been shown to increase pathological complete response (pCR) when used as neoadjuvant therapy.
Immunotherapy
Immunotherapy research in cancer has increased in recent years. Although most breast cancers respond poorly, some TNBCs have high tumor mutational burden (TMB) and many tumor-infiltrating lymphocytes (TILs), making them suitable for immune checkpoint inhibitor therapy. Recently, the FDA approved atezolizumab with nab-paclitaxel for treating metastatic or unresectable PD-L1–positive TNBC.
Related Article:
Invasive Breast Cancer
Non-Invasive Breast Cancer
Breast Cancer: How to Recognize Early Signs & Get Treatment
References:
Chen, Ziqi, et al. “Classifications of triple-negative breast cancer: insights and current therapeutic approaches.” Cell & Bioscience 15.1 (2025): 13.
Xu, Lili, et al. “Advancements in clinical research and emerging therapies for triple-negative breast cancer treatment.” European Journal of Pharmacology 988 (2025): 177202.
Obidiro, Onyinyechi, Gantumur Battogtokh, and Emmanuel O. Akala. “Triple negative breast cancer treatment options and limitations: future outlook.” Pharmaceutics 15.7 (2023): 1796.